A 55-year-old woman with a history of high blood pressure and chronic obstructive pulmonary disease (COPD) presented a clinical case that highlights the importance of recognizing dermatological conditions with systemic implications in a primary care setting. She was a smoker, consuming around ten cigarettes daily, had no known allergies, and was taking enalapril for six years and inhaled formoterol for the past two years.

Following a decline in her pulmonary condition, her pulmonologist modified her treatment by stopping formoterol and prescribing inhaled indacaterol combined with glycopyrronium. On the second day of using the new inhaler, she visited the primary care clinic due to painful, red patches that had developed on her cheeks and neck, accompanied by a low-grade fever. The patient denied any changes in diet or the use of new skincare products and mentioned some sun exposure but stated she used appropriate protection. She also reported no recent respiratory infections or cold symptoms. Given the sudden and unusual presentation of skin lesions, she was urgently referred to dermatology. The dermatologist recommended stopping the new inhaler and ordered a skin biopsy along with comprehensive blood tests, including a full blood count, autoimmune antibodies, lupus anticoagulant, and serology.
She was also started on oral corticosteroids. Within 24 to 48 hours of treatment, her symptoms began to subside significantly—pain lessened and the redness started to fade. Lab tests showed elevated white blood cell counts, particularly neutrophils, while antibody tests, lupus anticoagulant, and serology all returned negative. Approximately twenty days later, the skin biopsy confirmed the diagnosis of Sweet syndrome, a rare condition also known as acute febrile neutrophilic dermatosis. Histologically, Sweet syndrome is characterized by a dense infiltrate of neutrophils in the skin tissue.
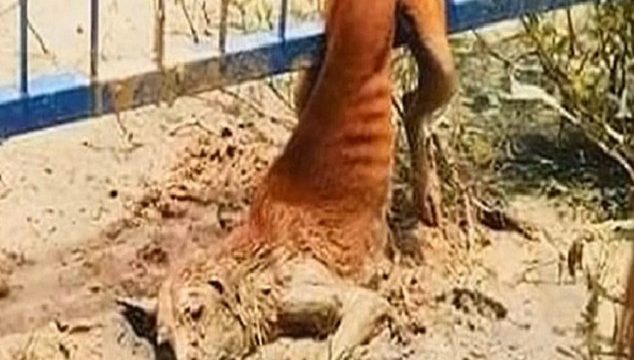
Clinically, it manifests as the abrupt onset of painful, red papules or plaques that often appear in an asymmetrical and bilateral pattern, mainly on the face, neck, upper chest, and hands. These lesions are commonly accompanied by systemic symptoms such as fever and neutrophilic leukocytosis. While the exact cause of Sweet syndrome remains unclear, it is believed to be triggered by cytokine-mediated immune responses that activate neutrophils and histiocytes. The syndrome can be associated with prior infections, malignancies, autoimmune diseases, and, notably, medications.
In this case, the onset of symptoms following the change in inhalation therapy strongly suggests a drug-induced reaction, even though there are no prior reports linking indacaterol-glycopyrronium to Sweet syndrome, making this case the first of its kind. Sweet syndrome is more frequently seen in women when the cause is idiopathic or drug-related. Drugs known to be associated with Sweet syndrome include contraceptives, certain antiepileptics, antibiotics, antihypertensives, colony-stimulating factors, and some vaccines. However, the list continues to grow, and clinicians must be open to suspecting other potential triggers. The first-line treatment for Sweet syndrome is oral corticosteroids, which usually produce rapid improvement, with general symptoms and skin lesions often resolving within a few days. Because the appearance of the lesions can mimic other conditions such as urticaria, contact dermatitis, drug eruptions, or even cutaneous lupus, differential diagnosis is essential. In this case, all other potential causes were ruled out through a thorough patient history and diagnostic tests, confirming Sweet syndrome. Given that Sweet syndrome can also involve internal organs and be a sign of underlying serious conditions like infections, hematologic malignancies, or autoimmune diseases, a complete systemic workup is necessary once the diagnosis is confirmed. For primary care providers, it’s vital to recognize such rare diseases, even when a definitive diagnosis isn’t immediately possible, because early referrals and accurate diagnoses rely heavily on clinical suspicion. Awareness of rare dermatologic syndromes like Sweet syndrome enables timely and appropriate care, potentially preventing complications. This case underscores the importance of considering a wide range of diagnoses and being alert to new medication-related reactions, even with drugs not previously associated with such effects.